Background: Telomeres are involved in maintenance of genomic stability and DNA repair. Telomeres of hematopoietic cells shorten with age, and accelerated telomere shortening is seen with replicative stress, such as during administration of chemotherapy for the treatment of cancer. We aimed to analyze leukocyte relative telomere length (RTL) among survivors of childhood hematologic malignancies, and to evaluate the associations of RTL with disease characteristics, treatment, and chronic health conditions (CHCs).
Method: This study was conducted at a single center in a retrospective cohort of survivors of childhood cancer diagnosed between 2000 and 2021 with a longitudinal follow-up of ≥1 year after cessation of treatment. The peripheral blood samples were collected between June 2022 and January 2023. This study enrolled survivors of childhood hematologic malignancies with the following criteria: diagnosis before the age of 19 years, continuous maintenance of clinical remission, compliance with regular clinical follow-up, and cessation of treatment more than one year before the start of the study. Considering that telomeres shorten with age, this study limited participants to those between 18 and 35 years of age at blood sampling. The telomere PNA Kit/Fluorescein isothiocyanate (FITC) for flow cytometry (Agilent Technologies, Singapore) was used for flow FISH for the measurement of leukocyte RTL.
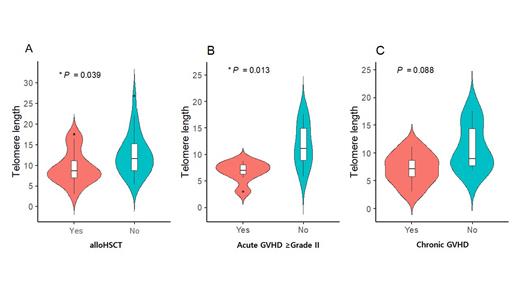
Result: Forty-three survivors of childhood hematologic malignancies with a median follow-up period of 73 months were recruited. Median age at diagnosis and at DNA sampling were 13.8 years (range, 6-18) and 22.6 years (range, 15-34), respectively. Survivors had leukemia (57.1%), lymphoma (31.4%), and myelodysplastic syndrome (11.4%). RTL in survivors of pediatric hematologic malignancies was not significantly shorter than the predicted value for age-matched references. There was no difference in RTL according to disease subtypes ( p=0.35). Survivors who experienced relapse had significantly shorter RTL than those who did not (7.6 ± 1.0 vs. 12.1 ± 5.0, p=0.009). Those who underwent allogeneic hematopoietic stem cell transplantation (HSCT) showed significant shortening of the RTL compared with those who did not (9.4 ± 4.1 vs. 12.6 ± 5.1, p=0.039). Total body irradiation (TBI) during pre-transplant conditioning did not influence the RTL (9.5 ± 3.8 with TBI vs. 12.1 ± 5.1 without TBI, p=0.117). Among the 15 patients who underwent allogeneic HSCT, those who developed acute graft-versus-host disease (GVHD) of grade II or higher had significantly shorter RTL than those who did not (6.8 ± 1.9 vs. 11.7 ± 4.1, p=0.013). Patients with chronic GVHD tended to have shorter RTL than those without GVHD, but the p-value was not statistically significant (7.1 ± 2.8 vs. 10.9 ± 4.2, p=0.088).
Seventeen patients had CHCs, with 13 having grade I and 4 having grade II. Patients with grade II CHCs had significantly shorter RTL than those without CHCs or with grade I CHCs (7.1 ± 1.6 vs. 11.5 ± 5.3, p=0.041). When the influence of multiple CHCs on RTL was examined, survivors with ≥2 CHCs had shorter RTL, but this difference was not significant ( p=0.062).
Conclusion: The overall RTL in survivors of childhood hematologic malignancy was not significantly shorter than the predicted values for age-matched references. However, patients who received allogeneic HSCT showed RTL attrition compared to those who did not receive HSCT. In addition, those who had GVHD showed augmented RTL attrition. Patients with grade II CHCs had shorter RTL compared to patients without or with grade I CHCs. Although there is currently no consensus on the extent and clinical significance of accelerated shortening of the RTL, the RTL may be a potential biomarker for determining CHCs in childhood hematologic malignancies.
Disclosures
No relevant conflicts of interest to declare.